特色簡介
目前每年在美國接受立體定位放射手術治療的病人總數,已超越開顱手術的案例數,全球接受過加馬刀放射手術的病人數也已累績突破一百萬大關。「加馬刀」立體定位放射手術已成為腦瘤、異常血管病灶、三叉神經痛等腦疾非侵入性治療的優先選擇。
2017年12月本院引進國內加馬刀治療機(Gamma Knife ® IconTM),結合了電腦斷層及先端的影像導引技術,可於治療中即時校正病灶與治療計畫的誤差,使得治療更精準、降低週遭組織的輻射傷害,提升病人的安全性。此外,加馬刀增加了面罩固定式的選擇,提升病人治療時的舒適性。
治療方式
加馬刀(Gamma Knife Icon)是利用鈷六十產生192條加馬射線(γ-ray),經由精密的電腦運算配合立體定位影像治療計畫,聚焦在治療病灶上,產生的高能量破壞目標細胞,達到與外科手術相似的效果,而病灶週遭正常組織因為接受的輻射劑量低,受到的傷害小,僅有少部分會產生短暫腫脹的情形,出現此現象時亦可經由藥物治療緩解。因為加馬刀放射手術是高精密度、快速、高能量的放射治療,並不是真的開刀,所以病人治療時不需麻醉,也沒有術後疼痛及傷口癒合的問題。
- 治療優點
- 人性化面罩固定式:提升治療時的舒適性。
- 可分次治療體積較大的病灶。
- 提高病患安全性:治療中即時校正病灶與治療計畫的誤差,治療更精準、降低週遭組織的輻射傷害。
- 強化製作劑量計畫的電腦功能,結合電腦斷層及先端的影像導引技術,可避免位移,提高定位精準度。
- 無傷口、不需全身麻醉,縮短治療時間。
- 治療流程
[加馬刀立體定位放射手術治療流程詳細說明]
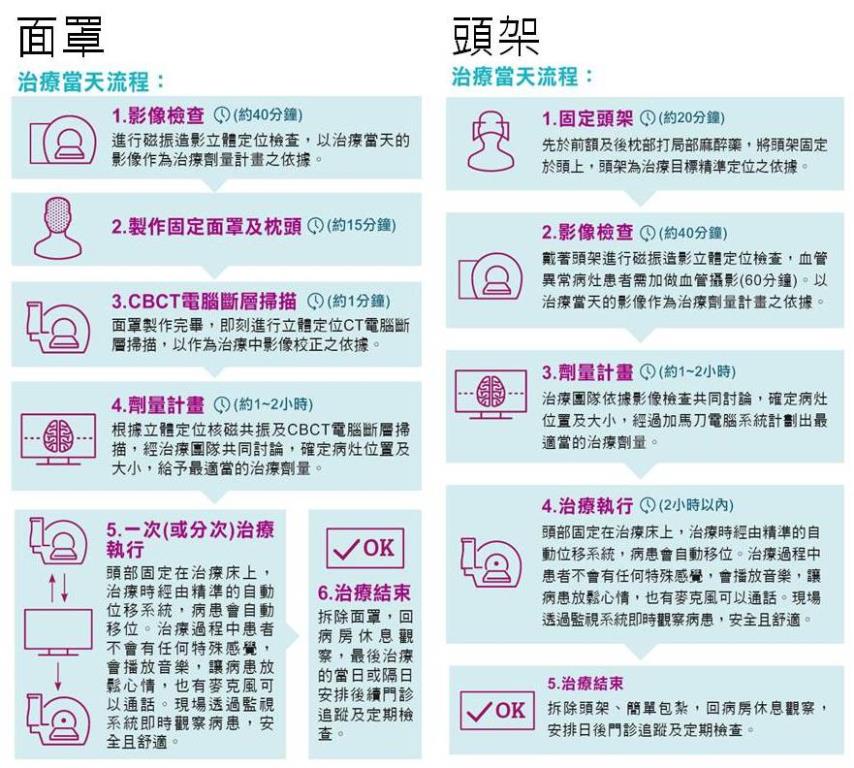
- [面罩]治療當天流程:
- 影像檢查(約40分鐘)
- 製作固定面罩及枕頭(約15分鐘)
- CBCT電腦斷層掃描(約1分鐘)
- 劑量計畫(約1~2小時)
- 一次(或分次)治療執行
- 治療結束
- [頭架]治療當天流程:
- 固定頭架(約20分鐘)
- 影像檢查(約40分鐘)
- 劑量計畫(約1~2小時)
- 治療執行(2小時以內)
- 治療結束
適用病症
加馬刀放射手術對於腦深部病灶、開顱術後殘餘或復發病灶,以及孩童、年紀大的長者或是無法承受手術及麻醉病患,為其替代治療選擇,並且可作為傳統全腦放射治療之協同或替代治療。適應症如下:
- 良性腦瘤:腦膜瘤、聽神經瘤、腦下垂體腫瘤、海綿竇血管瘤、顱咽瘤等。
- 血管異常病灶:腦動靜脈畸形、 動靜脈瘻管。
- 腦部轉移性腫瘤。
- 少數惡性腫瘤。
- 各種邊緣清楚且直徑小於3公分的腦瘤。
- 三叉神經痛。
- 其他功能性異常病患。
醫療團隊
- 神經外科劉斯顥醫師
- 神經外科周及人醫師
- 放射線部賴炳宏醫師
- 放射線部許碩修醫師
- 放射腫瘤部林裕為醫師
- 放射腫瘤部黃偉倫醫師
- 放射腫瘤部黃俞憲醫師
洽詢電話
連結網址
-----------------------------
Feature Introduction
Gamma Knife stereotactic radiosurgery has become the preferred non-invasive treatment for brain tumors, abnormal vascular lesions, trigeminal neuralgia, and other brain disorders. Currently, the annual number of patients receiving stereotactic radiosurgery in the United States has surpassed the number of craniotomy cases. Globally, the number of patients who have undergone Gamma Knife radiosurgery has exceeded one million.
In December 2017, our hospital introduced a new Gamma Knife treatment model (Gamma Knife® Icon™), which combines computed tomography and advanced image-guided technology. This model allows for real-time correction of discrepancies between the lesion and the treatment plan during treatment, enhancing precision, reducing radiation exposure to surrounding tissues, and improving patient safety. Additionally, the new Gamma Knife system has added a mask fixation option, improving patient comfort during treatment.
Treatment Method
The Gamma Knife uses 192 gamma-ray beams produced by cobalt-60. Through precise computer calculations combined with stereotactic imaging treatment planning, it focuses on the treatment lesion, generating high energy to destroy target tumor cells, achieving effects similar to surgical procedures. The surrounding normal tissues receive a low radiation dose, resulting in minimal damage, with only a small portion experiencing temporary swelling, which can be alleviated through medication when it occurs. Because Gamma Knife radiosurgery is a high-precision, rapid, high-energy radiation treatment and not actual surgery, patients do not require anesthesia and have no issues with post-operative pain or wound healing.
A. Treatment Advantages
I. Customized mask fixation: Enhances comfort during treatment.
II. Ability to treat larger lesions in several fractions.
III. Improved patient safety: Real-time correction of errors between the lesion and treatment plan during treatment, making treatment more precise and reducing radiation damage to surrounding tissues.
IV. Enhanced computer functionality for dose planning, combining CT and advanced image-guided technology to avoid displacement and improve positioning accuracy.
V. Non-invasive, no general anesthesia required, shortened treatment time.
B. Treatment Process [Detailed explanation of the Gamma Knife stereotactic radiosurgery treatment process]
I. [Mask-Based] Treatment procedure:
- Imaging examination (about 40 minutes)
- Creating a fixation mask and pillow (about 15 minutes)
- CBCT scan (about 1 minute)
- Dose planning (about 1-2 hours)
- Single (or fractionated for several days) treatment execution
- Treatment completion
II. [Frame-Based] Same-day treatment procedure:
- Head frame fixation (about 20 minutes)
- Imaging examination (about 40 minutes)
- Dose planning (about 1-2 hours)
- Treatment execution
- Treatment completion
Applicable Conditions
Gamma Knife radiosurgery is an alternative treatment option for deep brain lesions, residual or recurrent lesions after craniotomy, as well as for children, elderly patients, or those unable to tolerate surgery and anesthesia. It can also serve as an adjunctive or alternative treatment to conventional whole-brain radiotherapy. The conditions suitable for Gamma Knife treatment include:
A. Benign brain tumors: Such as meningiomas, acoustic neuromas, pituitary tumors, cavernous sinus hemangiomas, craniopharyngiomas, etc.
B. Vascular abnormalities: cerebral arteriovenous malformations (AVMs), arteriovenous fistulas.
C. Brain metastases.
D. Certain malignant tumors.
E. Various brain tumors with clear margins and diameters less than 3 cm.
F. Trigeminal neuralgia.
G. Other functional disorders.